Timing of Medication
Introduction
I have encountered some patients who asked about the appropriate timing for taking their oral medication (morning, afternoon or night) when they were advised to take it once a day.
Generally, I inform them that the specific timing for taking the medicine is not crucial and they can select a suitable time that suits them best.
- More importantly, they should take the medications at the same time each day to establish a regular habit.
Below are some medications that require specific timing.
NOTE: Administration of medication before, with or after food is discussed at a separate post.
Chronotherapy
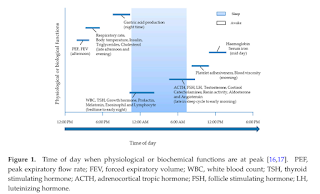
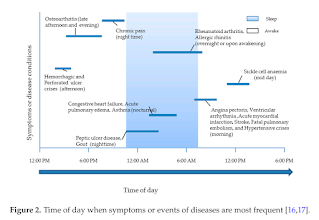
Chronotherapy involves the administration of medication in coordination with the body's circadian rhythms to maximise therapeutic effectiveness and minimise/avoid adverse effects.
- This is a promising aspect, but more extensive research is needed.
Medications that Cause Drowsiness
Logically, medications that can cause drowsiness, such as benzodiazepines, opioids, first-generation antihistamines (e.g. chlorpheniramine, dexchlorpheniramine, promethazine) and muscle relaxants, are recommended to take closer to bedtime if possible. If patients are affected, do not drive or operate machinery.
ADHD Medications
Stimulants (e.g. methylphenidate) and atomoxetine are often given in the morning to control symptoms.
Antidepressants
Dosing instructions for antidepressants vary depending on the specific drug. Selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, tricyclic antidepressants, and monoamine oxidase inhibitors can cause either activating or sedating adverse reactions. Administer activating drugs in the morning and sedating drugs in the evening to avoid insomnia or daytime drowsiness, respectively. Some adverse reactions can be used as an advantage. For example, amitriptyline has sedative effects and may help patients sleep.
- Morning: Escitalopram, fluoxetine, moclobemide, sertraline,
- Bedtime: Agomelatine, fluvoxamine, mirtazapine, paroxetine, TCAs
Antihypertensive Drugs
As an overview, blood pressure follows a circadian rhythm, with BP levels falling during sleep and increasing in the early morning hours in most individuals. In patients with hypertension, a lack of fall in night-time BP (i.e. nondipping) and/or marked rise or surge in BP during the early morning hours is associated with a higher incidence of stroke and an increased risk for other cardiovascular complications, especially among the elderly.
In some studies, shifting at least one antihypertensive medication from the morning to the evening both restored the normal nocturnal blood pressure dip and reduced 24-hour mean blood pressure.
- Changing the Timing of Antihypertensive Therapy to Reduce Nocturnal Blood Pressure in CKD: An 8-week Uncontrolled Trial, 2007
- Administration Time-Dependent Effects of Valsartan on Ambulatory Blood Pressure in Elderly Hypertensive Subjects, 2005
- Chronotherapy Improves Blood Pressure Control and Reverts the Nondipper Pattern in Patients With Resistant Hypertension, 2008
- Evening Versus Morning Dosing of Antihypertensive Drugs in Hypertensive Patients With Sleep Apnoea: A Cross-Over Study, 2015
- Bedtime Hypertension Treatment Improves Cardiovascular Risk Reduction: The Hygia Chronotherapy Trial, 2019
- A Trial of 2 Strategies to Reduce Nocturnal Blood Pressure in Blacks With Chronic Kidney Disease, 2013
- Time of administration important? Morning versus evening dosing of valsartan, 2015
- Differential Effects of Morning and Evening Dosing of Nisoldipine ER on Circadian Blood Pressure and Heart Rate, 1999
- Randomized Crossover Trial of the Impact of Morning or Evening Dosing of Antihypertensive Agents on 24-Hour Ambulatory Blood Pressure, 2018
As shown above, the evidence on antihypertensive best administration time is actually in a mix. My personal stance is to take the antihypertensive medications consistently at a time (morning or night), do not keep on changing. If patient experienced dizziness post multiple antihypertensive medications, it might be a good idea to separate the administration time.
Aspirin for Preeclampsia
Bedtime administration of low dose aspirin (75 mg-150 mg) starting at 12-16 weeks gestation appears to be associated with greater protection from preeclampsia compared with administration in the morning.
Bisphosphonates
Because food may prevent absorption, oral bisphosphonates (e.g. alendronate, risedronate) should be taken in the morning, 30 to 60 minutes before breakfast.
- Following administration, they should remain upright until after breakfast to avoid oesophageal or gastric irritation.
Diuretics
By altering the body's electrolyte composition, especially sodium, diuretics influence the amount of urine production. Teach patients to take these medication (e.g. hydrochlorothiazide, indapamide, spironolactone, bumetanide, frusemide) in the morning or early afternoon to avoid nocturia and subsequent sleep interruptions.
H2 Receptor Antagonists
Bedtime dosing can help reduce overnight symptoms such as heartburn. Night-time acid secretion is primarily mediated by histamine.
Isosorbide Dinitrate
Nitrate tolerance has been a major problem with the use of nitrates as chronic antianginal therapy. As suggested in Lexicomp, the administration of isosorbide dinitrate should not be around the clock, but to allow nitrate-free interval of at least 14 hours for immediate release products and at least 18 hours for sustained release products.
- Immediate release products: For twice daily dosing, consider administering at 8 am and 1 pm. For 3 times daily dosing, consider 8 am, 1 pm and 6 pm.
- Sustained release products: Consider once daily in morning or twice-daily dosing at 8 am and between 1 pm and 2 pm.
Levothyroxine
To improve drug absorption, administer consistently in the morning on an empty stomach, at least 30 to 60 minutes before food. Alternatively, may consistently administer at night 3 to 4 hours after the last meal. Do not administer within 4 hours of calcium- or iron-containing products.
Oral Contraceptive Pills
It is very important to take oral contraceptive pills at the same time each day. If there is a missed dose, the contraceptive efficacy may be affected.
Prostaglandin Analogues for Glaucoma at Night
In open-angle glaucoma management, prostaglandin analogues (e.g. bimatoprost, latanoprost, tafluprost and travaprost) are typically first-line therapy. Because the medications take about 2 weeks to achieve their maximum therapeutic effect, follow-up for efficacy should occur no sooner than 2 weeks.
They are typically dosed only ONCE a day, preferably at evening for optimal effect:
- After 6 months, latanoprost applied in the morning reduced diurnal IOP from 25.5 to 17.7 mm Hg (31%) and latanoprost applied in the evening, from 24.8 to 16.2 mm Hg (35%).
- Both morning and evening dosings of travoprost provide effective 24-hour IOP reduction. However, the evening dosing of travoprost demonstrates slightly greater daytime efficacy, with a narrower range of 24-hour pressure.
Statins
At outpatient pharmacy, we often counsel patients to take statins at night. However, this statement is not universally applicable to all statins available in the market. It is rather a simplified way of remembering the dosing time and subsequently, improves patient compliance.
- The shorter-acting statins, pravastatin and simvastatin, may slightly more effective if taken at bedtime compared to morning due to increased cholesterol production overnight when there is less food in the stomach.
- However, rosuvastatin and atorvastatin, can be taken at any time of the day due to their long time of action.
Warfarin
Take warfarin tablets at approximately the same time each day. Most people take their daily warfarin dose in the evening. This allows the dose to be changed if necessary on the day that an INR result is obtained, rather than waiting until the next day.
Others
Morning- Canagliflozin - Take preferably before the 1st meal of the day.
- Doxazosin Extended-Release Tablet - with morning meals
- Ertugliflozin
- Gliclazide MR Tablet - with breakfast
- Moxonidine
- Neratinib
- Tacrolimus Prolonged Release Capsule - on empty stomach
- Vastarel 80 mg XR Capsule - during breakfast
- Vildagliptin - when used once daily dosing
Evening
- Adapalene 0.1% and Benzoyl Peroxide 2.5% Gel (Epiduo)
- Clindamycin 1% and Benzoyl Peroxide 5% Gel (Duac)
- Lixisenatide
- Lurasidone
- Metformin XR - with evening meals
- Montelukast
- Rivaroxaban - with evening meals for nonvalvular atrial fibrillation
Bedtime
- Adapalene 0.1% cream or gel
- Ciclosporin 0.1% ophthalmic emulsion (Ikervis)
- Donepezil
- Efavirenz - on empty stomach
- Fluocinolone Acetonide 0.01%, Hydroquinone 4% and Tretinoin 0.05% Cream (Tri-Luma) - at least 30 min before bedtime
- Fosfomycin
- Imiquimod 5% cream
- Lemborexant
- Perampanel
- Senna
- Strontium ranelate
- Thalidomide - take at least 1 hour after food and preferably at night to avoid feeling sleepy during the day
External Links
- Additional bedtime H2-receptor antagonist for the control of nocturnal gastric acid breakthrough, 2009
- Timing When to Take Your Daily Medications, 2013
- Timing of Administration: For Commonly-Prescribed Medicines in Australia, 2016
- Chronotherapy with low-dose aspirin for prevention of complications in pregnancy, 2013
- Levothyroxine: More Leeway In Timing of Administration?, 2018
- What time of day should I take my medicine?, 2019
- Does it really matter when you take medication?, 2019
- Timely Medication Administration Guidelines, 2019
May I know why T. Metformin XR need to be taken with evening meal instead of in the morning?
ReplyDeleteMetered release of metformin from the tablet and administration with the evening meal when gastric residence time is at its longest are thought to be factors in explaining better tolerability than IR formulation.
DeleteAlso, Metformin XR is taken after evening meals to optimize the suppression of hepatic gluconeogenesis at night.
Delete