Pharmaceutical Care Issues
Introduction
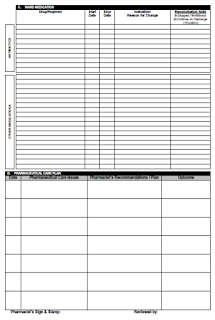
Case clerking using CP2 (Pharmacotherapy Review) form and medication review are often done concurrently.
- If the pharmaceutical case issue is significant to the patient's current medical plan, the issue should be highlighted to other healthcare providers during ward rounds or whenever necessary.
Prior Starting
First, we should make a comprehensive medication management review.
- Summary of all relevant past and current medical conditions
- Chief complaint - The reason patient is seeking medical care, documented in patient's own words.
- History of presenting illness - Description on progression of patient's current problem.
- Past medical history
- Reason for use of each medicine.
- All current medicines (including prescription, non-prescription and complementary medicines), compliance aids, therapeutic devices and appliances
- Medication history, including immunisations
- Dose, strength, dose form, directions, route of administration, duration of therapy and indication for use for each medicine, with any special medicine administration instructions.
- When-necessary ("prn") medicines and the frequency of their administration.
- Short-term medicines (e.g. antibiotic courses)
- Relevant observations and notes on symptoms and signs at the time of review
- E.g. Blood pressure, respiratory rate, pulse rate, temperature, random blood sugar, oxygen saturation
- Relevant pathology result
- Discuss the patient's health-related concerns, beliefs, attitudes and preferences
- Consider the patient's quality of life and life expectancy
- Provide education and support to the patient and their carer
Identifying Medication-related Problems
Are all the existing health problems well managed with medicines?
- Identify if there is any untreated indication.
- Constipation due to opioids
- Review the pharmacotherapy management with latest guidelines
Are therapeutic objectives being achieved (symptom control and prevent disease progression)?
- Antibiotics - CRP, WBC, Temperature
- Antihypertensives - Blood pressure
- Antidiabetics - Blood sugar level
- Antiepileptics - Seizure history and therapeutic drug monitoring
Is there a documented reason or evidence base for use of a medicine?
- Identify any medication use without indication or unnecessary medicine (e.g. medicine for a medical condition that has resolved).
- Benzodiazepines
- Proton pump inhibitors
- Analgesics
- Antibiotics
- Therapeutic duplication
- Identify if there is any subtherapeutic or overdosage of correct medicine.
- Identify if there is any contraindicated medicine?
- Consider antimicrobial stewardship and Intravenous Antibiotics-Oral Switch Therapy.
- Drug administration error?
Are there any patient-specific issues that will affect use of the medicine?
- Allergy/drug sensitivity
- Patient inhalers and insulin injection technique
- Patient adherence to medication?
- Is the dosing schedule convenient?
- Is the medicine in a form the patient can take? Swallowing difficulty or Ryle's tube feeding?
- Cost of medications
- Patient renal profile - Renal dose adjustment?
- Patient is a paediatric - Double check if drugs are dosed correctly
- Patient is an elderly - Consider AGS Beers criteria and any prescribing cascades
- Patient is obese - Consider dose adjustment
- Patient is pregnant or breastfeeding - Consider drug safety
- Patient is G6PD Deficiency - Consider drug safety
What risks are associated with use of the medicine, and what monitoring is required?
- Identify if any drug interactions
- Look for adverse drugs reactions
- Review laboratory data (including any increasing or decreasing trend)
- Liver function test if patient has liver problem, e.g. liver cirrhosis, hepatitis
- Drug monitoring post initiation
- ACE inhibitors - renal profile (including potassium level), blood pressure and dry cough
- Warfarin - INR
- Gentamicin, vancomycin, phenytoin, sodium valproate, carbamazepine, digoxin - Consider therapeutic drug monitoring
Pharmaceutical Care Plan
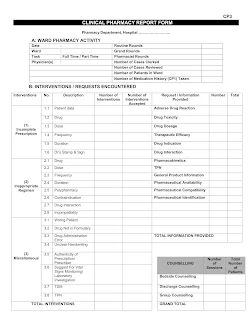
Identified pharmaceutical care issues shall be described based on the Clinical Pharmacy Report Form (CP3) in the following format.
- PCI: Description of PCI which clearly reflect pharmacotherapy suggestion to be made.
- Pharmacist's recommendations/plan: Suggestion made to the doctor.
- Outcome: Patient oriented outcome following intervention. If outcome is unable to be observed on the same day, may write a monitoring plan.
Example:
- PCI: 2.1 Inadequate drug. BP persistently high (158/70 mm Hg) since admission.
- Pharmacist's recommendation: To restart T. amlodipine 5 mg OD (Target BP <140/80 mm Hg).
- Outcome:
- If outcome is available: T. Amlodipine initiated. BP controlled at 138/ 60 mm Hg.
- If outcome is unable to be observed: Monitor BP daily. Target BP < 140/80 mm Hg.
External Links
- PSA - Medication Management Guidelines
- Malaysian Pharmacists’ Involvement in Pharmaceutical Care: A Narrative Review, 2019
- Pharmacists’ Interventions on Electronic Prescriptions from Various Specialty Wards in a Malaysian Public Hospital: A Cross-Sectional Study, 2021
- Guideline on Ward Pharmacy Activities, 2023

Comments
Post a Comment